The Diabetes Mellitus Type 2 Concept Map provides a comprehensive overview of this prevalent condition, exploring its pathophysiology, diagnosis, management, complications, and emerging therapies. This detailed resource offers a thorough understanding of diabetes mellitus type 2, empowering healthcare professionals and individuals alike to make informed decisions regarding its prevention and management.
The second paragraph delves into the intricacies of diabetes mellitus type 2, unraveling its complex mechanisms and highlighting the significance of early detection, effective management, and ongoing research in combating this global health concern.
Pathophysiology of Diabetes Mellitus Type 2
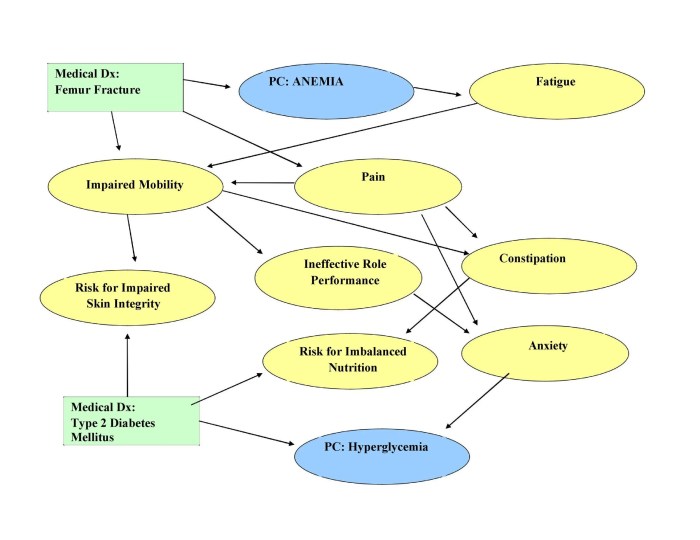
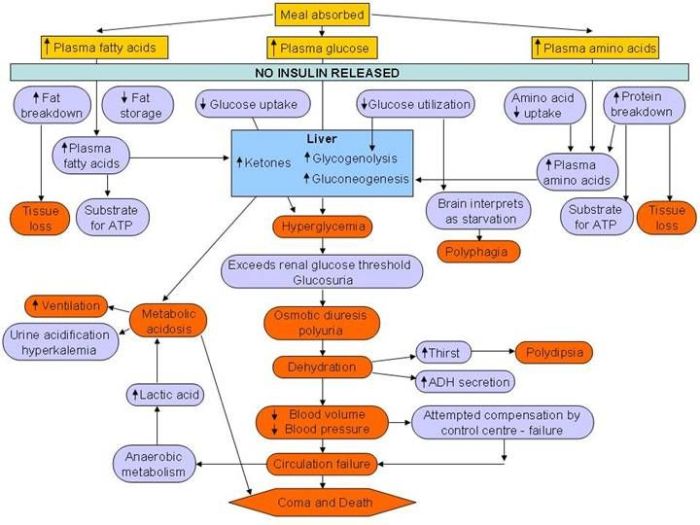
Type 2 diabetes mellitus (T2DM) is a metabolic disorder characterized by chronic hyperglycemia due to insulin resistance and impaired insulin secretion. Understanding the pathophysiology of T2DM is crucial for effective management and prevention.
Genetic and Environmental Factors
Genetic predisposition plays a significant role in T2DM, with a complex interplay of genetic variants contributing to insulin resistance and beta-cell dysfunction. Environmental factors, such as obesity, sedentary lifestyle, and unhealthy diet, further interact with genetic susceptibility, increasing the risk of developing T2DM.
Insulin Resistance and Impaired Glucose Metabolism
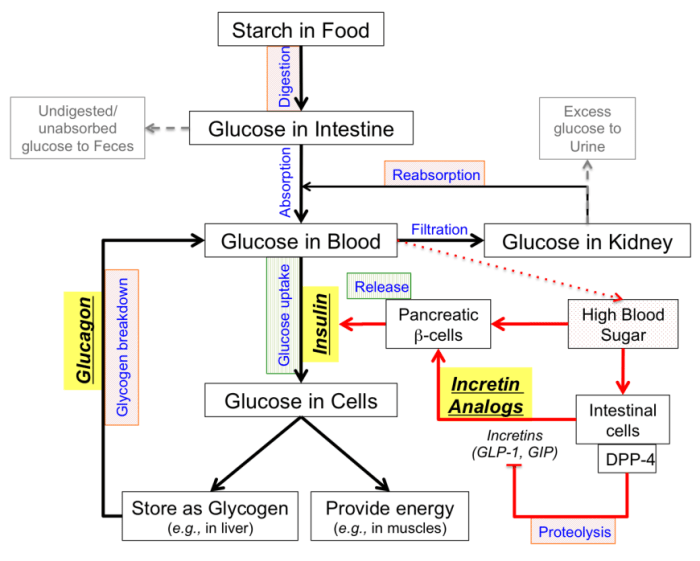
Insulin resistance is a hallmark of T2DM, where tissues such as muscle, liver, and fat become less responsive to insulin’s actions. This results in impaired glucose uptake and utilization, leading to elevated blood glucose levels (hyperglycemia).
In T2DM, the pancreas initially compensates for insulin resistance by increasing insulin secretion. However, over time, beta-cells become dysfunctional and fail to produce sufficient insulin, leading to a further decline in glucose metabolism and persistent hyperglycemia.
Metabolic Consequences of Hyperglycemia
Chronic hyperglycemia has detrimental effects on various organs and tissues, contributing to the development of microvascular and macrovascular complications:
- Microvascular complications:Hyperglycemia damages small blood vessels, leading to retinopathy, nephropathy, and neuropathy.
- Macrovascular complications:Hyperglycemia promotes atherosclerosis, increasing the risk of cardiovascular events such as heart attack and stroke.
Diagnosis and Monitoring of Diabetes Mellitus Type 2

Accurate diagnosis and ongoing monitoring are crucial for effective management of type 2 diabetes. This section will explore the diagnostic criteria, screening guidelines, and various laboratory tests used to assess and monitor glycemic control.
Diagnostic Criteria and Screening Guidelines
The diagnosis of type 2 diabetes is based on specific criteria established by reputable organizations such as the American Diabetes Association (ADA) and the World Health Organization (WHO). These criteria include:
- Fasting plasma glucose (FPG):A fasting blood glucose level of 126 mg/dL (7.0 mmol/L) or higher on two separate occasions.
- Oral glucose tolerance test (OGTT):A two-hour blood glucose level of 200 mg/dL (11.1 mmol/L) or higher after ingesting a standardized glucose solution.
- Glycated hemoglobin (HbA1c):An HbA1c level of 6.5% or higher.
- Random plasma glucose:A random blood glucose level of 200 mg/dL (11.1 mmol/L) or higher in the presence of classic symptoms of diabetes (e.g., polyuria, polydipsia, unexplained weight loss).
Screening guidelines recommend that all adults over the age of 45 be screened for type 2 diabetes. Individuals with certain risk factors, such as obesity, family history of diabetes, or physical inactivity, may benefit from earlier screening.
Laboratory Tests for Glycemic Control
Regular monitoring of blood glucose levels is essential for managing type 2 diabetes and preventing complications. Several laboratory tests are used for this purpose:
- Fasting plasma glucose (FPG):Measures the blood glucose level after an overnight fast.
- Postprandial glucose:Measures the blood glucose level two hours after a meal.
- Glycated hemoglobin (HbA1c):Reflects the average blood glucose level over the past 2-3 months.
- Continuous glucose monitoring (CGM):Provides real-time glucose readings throughout the day and night.
HbA1c is considered the gold standard for assessing long-term glycemic control and is used to set treatment goals. The ADA recommends an HbA1c target of less than 7% for most people with type 2 diabetes.
Importance of Regular Monitoring
Regular monitoring of blood glucose levels allows individuals with type 2 diabetes to:
- Assess the effectiveness of their treatment plan.
- Identify patterns and trends in their blood glucose levels.
- Make necessary adjustments to their medication, diet, or lifestyle.
- Prevent or delay the development of complications, such as cardiovascular disease, neuropathy, and retinopathy.
Management of Diabetes Mellitus Type 2: Diabetes Mellitus Type 2 Concept Map
The management of type 2 diabetes mellitus involves a multidisciplinary approach that encompasses lifestyle modifications, pharmacological therapy, patient education, self-management, and adherence to treatment plans. This comprehensive approach aims to control blood glucose levels, prevent complications, and improve overall health and well-being.
Lifestyle Modifications
Lifestyle modifications play a crucial role in managing type 2 diabetes. These include:
- Diet:A healthy diet that is low in refined carbohydrates, sugary drinks, and unhealthy fats can help control blood glucose levels and promote weight loss.
- Exercise:Regular physical activity can improve insulin sensitivity and lower blood glucose levels.
- Weight management:Maintaining a healthy weight can reduce insulin resistance and improve overall metabolic health.
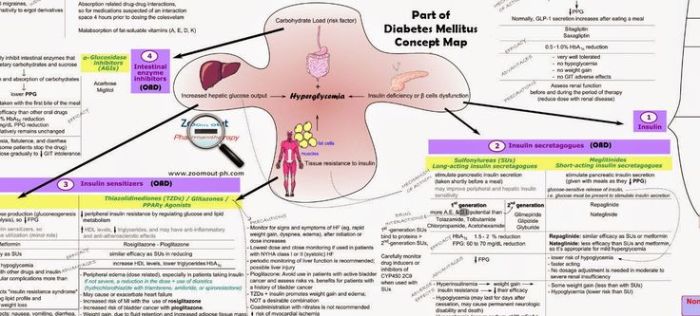
Pharmacological Therapy
Pharmacological therapy may be necessary to control blood glucose levels in people with type 2 diabetes. Medications used include:
- Oral medications:These include metformin, sulfonylureas, and thiazolidinediones, which work by increasing insulin sensitivity, stimulating insulin secretion, or reducing glucose production.
- Injectable agents:These include GLP-1 agonists and SGLT2 inhibitors, which can lower blood glucose levels by increasing insulin secretion, slowing gastric emptying, or promoting glucose excretion in the urine.
- Insulin:Insulin therapy may be necessary for people with type 2 diabetes who cannot achieve adequate blood glucose control with other medications.
Patient Education, Self-Management, and Adherence
Patient education, self-management, and adherence to treatment plans are essential for successful diabetes management. This includes:
- Patient education:Patients need to understand their condition, treatment options, and lifestyle modifications to effectively manage their diabetes.
- Self-management:Patients should be able to monitor their blood glucose levels, adjust their medications, and make healthy lifestyle choices.
- Adherence to treatment plans:Patients need to take their medications as prescribed, follow dietary recommendations, and engage in regular physical activity to achieve optimal outcomes.
Complications of Diabetes Mellitus Type 2
Diabetes mellitus type 2 is a chronic metabolic disorder characterized by hyperglycemia, which can lead to a range of acute and chronic complications affecting various organs and systems.
Early detection, screening, and preventive measures are crucial to minimize the risk of these complications and improve the overall health and well-being of individuals with type 2 diabetes.
Microvascular Complications
Microvascular complications arise from damage to small blood vessels, particularly in the eyes, kidneys, and nerves.
- Retinopathy: Damage to the blood vessels in the retina can lead to vision impairment, blindness, and even retinal detachment.
- Nephropathy: Damage to the blood vessels in the kidneys can impair kidney function, leading to chronic kidney disease and end-stage renal failure.
- Neuropathy: Damage to the nerves can cause numbness, tingling, pain, and weakness in the extremities, particularly in the feet and hands.
Risk factors for microvascular complications include poor glycemic control, hypertension, dyslipidemia, and smoking.
Cardiovascular Complications
Diabetes mellitus type 2 is a major risk factor for cardiovascular disease, including:
- Coronary artery disease: Narrowing of the arteries that supply blood to the heart, increasing the risk of heart attack.
- Stroke: Blockage or rupture of blood vessels in the brain, leading to brain damage or death.
- Peripheral artery disease: Narrowing of the arteries in the legs and feet, causing pain, numbness, and impaired circulation.
Risk factors for cardiovascular complications in diabetes include poor glycemic control, hypertension, dyslipidemia, obesity, and smoking.
Other Complications
- Skin infections: Diabetes impairs the immune system, making individuals more susceptible to skin infections, such as cellulitis and abscesses.
- Foot ulcers: Nerve damage and poor circulation in the feet can lead to foot ulcers, which can become infected and difficult to heal.
- Gastroparesis: Damage to the nerves in the stomach can slow down digestion, causing nausea, vomiting, and abdominal pain.
Emerging Therapies and Research in Diabetes Mellitus Type 2
The management of type 2 diabetes has witnessed significant advancements in recent years, with the emergence of novel therapeutic strategies and cutting-edge technologies. These advancements aim to improve glycemic control, prevent complications, and ultimately find a cure for this prevalent condition.
Pharmacological Innovations
Novel pharmacological agents have played a pivotal role in the treatment of type 2 diabetes. Glucagon-like peptide-1 (GLP-1) agonists, sodium-glucose cotransporter 2 (SGLT2) inhibitors, and dipeptidyl peptidase-4 (DPP-4) inhibitors are among the most promising agents.
- GLP-1 agonists mimic the action of the incretin hormone GLP-1, stimulating insulin secretion and suppressing glucagon release, thereby improving glycemic control.
- SGLT2 inhibitors block the reabsorption of glucose in the proximal tubules of the kidneys, leading to increased glucose excretion in the urine and reduced blood glucose levels.
- DPP-4 inhibitors prolong the action of incretin hormones, enhancing insulin secretion and reducing glucagon release.
Technological Advancements, Diabetes mellitus type 2 concept map
Emerging technologies have revolutionized the monitoring and management of type 2 diabetes.
- Continuous glucose monitoring (CGM) systems provide real-time glucose readings, allowing individuals to closely monitor their blood sugar levels and make informed decisions about insulin dosing and lifestyle modifications.
- Artificial pancreas systems combine CGM with an insulin pump, automating insulin delivery based on real-time glucose levels, improving glycemic control and reducing the burden of diabetes management.
- Personalized medicine approaches utilize genetic and other individual-specific data to tailor treatment plans, optimizing outcomes and minimizing adverse effects.
Ongoing Research
Research efforts are continuously underway to further improve the management and treatment of type 2 diabetes.
- Researchers are investigating the use of stem cell therapy to regenerate pancreatic beta cells, restoring insulin production and potentially curing diabetes.
- Studies are exploring the role of bariatric surgery in the remission of type 2 diabetes, with promising results in certain individuals.
- Ongoing clinical trials are evaluating the efficacy and safety of new pharmacological agents and combination therapies.
Essential Questionnaire
What is the primary mechanism underlying diabetes mellitus type 2?
Insulin resistance, characterized by the body’s inability to effectively utilize insulin, is the central mechanism in diabetes mellitus type 2.
How is diabetes mellitus type 2 diagnosed?
Diagnosis involves assessing fasting and postprandial glucose levels, hemoglobin A1c (HbA1c), and other laboratory tests to determine if glucose levels exceed established thresholds.
What are the key components of diabetes mellitus type 2 management?
Management encompasses lifestyle modifications (diet, exercise, weight management), pharmacological therapy (oral medications, injectable agents, insulin), patient education, self-management, and adherence to treatment plans.
What are the potential complications associated with diabetes mellitus type 2?
Complications include microvascular (retinopathy, nephropathy, neuropathy) and macrovascular (coronary artery disease, stroke, peripheral artery disease) events, highlighting the importance of early detection and preventive measures.